ATPL Brain Disease: Expert Diagnosis & Treatment
What is the nature of certain neurological conditions affecting aviators and their implications for flight safety?
Certain neurological disorders can impact an individual's ability to perform complex tasks, including piloting aircraft. These conditions may present with a wide range of symptoms, affecting cognitive functions, motor skills, and sensory perception. Examples include various types of cognitive impairment, movement disorders, and sensory processing difficulties. The specific impact on an aviator depends on the nature and severity of the condition, as well as the demands of the flight environment.
The safety implications of these conditions are significant. A pilot experiencing any form of neurological impairment may be unable to adequately respond to unexpected situations or maintain the required level of vigilance and coordination. Historical records show cases where neurological conditions, often undetected before a period of training or employment, later compromised flight safety. Proactive medical evaluations and comprehensive screening programs are essential in aviation to mitigate this risk. Furthermore, these conditions necessitate specialized management and support to ensure the well-being and potential return to flight of affected individuals, where appropriate.
- Zoe Spencer Net Worth 20242025 How Much Does She Earn
- Katy Perrys Daring Looks Topless Moments Latest Photos
The following sections will explore the diagnostic criteria, management strategies, and regulatory frameworks surrounding neurological health in aviation.
Neurological Conditions in Aviation
Assessing neurological health is crucial for aviation safety. Pilots must maintain optimal cognitive function, motor skills, and sensory perception. Conditions impacting these areas require careful evaluation and management.
- Diagnosis
- Treatment
- Symptom evaluation
- Cognitive function
- Motor skills
- Sensory perception
- Regulatory standards
- Pilot fitness
The eight key aspects illuminate the multifaceted nature of neurological health in aviation. Diagnosis relies on medical evaluations and assessments of cognitive function and motor skills. Treatment strategies must address the specific condition. Symptom evaluation is ongoing to identify changes and their impact. Motor skills assessments are necessary to understand functional ability. Cognitive impairment, a common issue, necessitates careful monitoring. Changes in sensory perception can affect piloting. Regulatory frameworks set standards for pilot fitness. These standards ensure competent pilots, mitigating risks associated with neurological conditions and guaranteeing flight safety.
- Coco Bliss Hot Pics Videos What You Need To Know
- Josh Allen Sean Mcdermott Contracts Salaries Bills Future
1. Diagnosis
Accurate diagnosis of neurological conditions impacting aviation personnel is paramount. A precise diagnosis underpins effective management strategies and ensures compliance with safety regulations. The process involves meticulous evaluation of presenting symptoms, medical history, and physical examinations. Neurological assessments, encompassing cognitive function tests and motor skill evaluations, are integral components. These assessments aim to identify subtle impairments that might not be immediately apparent but could nonetheless compromise flight safety. For instance, subtle deficits in spatial reasoning or reaction time, while not obvious in daily activities, could pose significant risks during critical phases of flight.
The importance of early and comprehensive diagnosis cannot be overstated. Conditions manifesting gradually, such as certain forms of dementia or progressive neurological disorders, may not exhibit noticeable symptoms during initial stages of development, but significant functional impairment can emerge over time. Regular medical evaluations, coupled with meticulous monitoring of pilot performance and specific tasks relevant to aviation, are critical to detect these potentially insidious developments. Detailed records of pilot performance and self-reported symptoms are essential in this context. These documented reports assist medical professionals in recognizing emerging trends and subtle shifts in cognitive or motor function that might indicate a developing neurological issue. Effective diagnosis fosters informed decision-making regarding pilot fitness for duty, enabling appropriate intervention and mitigating potential safety risks.
In conclusion, diagnosis plays a pivotal role in managing neurological conditions that might affect aviators. Early identification through comprehensive evaluations and ongoing monitoring is crucial for flight safety. Maintaining detailed records of medical assessments and performance data provides critical context for informed decisions about pilot fitness for duty. This proactive approach ensures the well-being of individuals and enhances the safety of air travel.
2. Treatment
Treatment for neurological conditions affecting aviators, while diverse, focuses on managing symptoms, mitigating the progression of the condition, and ensuring continued safety. The specific approach depends critically on the underlying cause and the nature of the condition. Treatment strategies may involve medications, lifestyle modifications, or therapies aimed at improving cognitive function and motor skills. Effective treatment aims to maintain the aviator's ability to perform essential tasks and navigate challenging situations, critical factors for ensuring flight safety.
The effectiveness of treatment often hinges on early intervention. Catching a condition early when it might still be amenable to treatment strategies can significantly influence long-term outcomes. For example, managing certain neurological conditions with appropriate medication and rehabilitation therapies can help maintain or improve cognitive functions and motor skills. This can be vital in the aviation context, where maintaining sharp focus, quick reflexes, and precise coordination are paramount. However, treatment alone may not always restore full function, highlighting the need for careful assessment and ongoing monitoring. Pilot retraining or reevaluation of duties might be necessary for conditions that significantly impact abilities required for flight. These adaptive measures help minimize risks associated with compromised performance while prioritizing both the pilot's safety and the safety of passengers.
In summary, the treatment of neurological conditions impacting aviators is complex and multifaceted. Appropriate intervention, often including medication, therapy, and lifestyle adjustments, aims to mitigate symptoms, prevent further deterioration, and ensure continued safety. The emphasis on early intervention and ongoing assessment is essential, given the varied and often unpredictable nature of these conditions. The impact of treatment, while valuable, is not always fully restorative, underscoring the importance of adaptive measures to support the safety of both the affected individual and the traveling public.
3. Symptom evaluation
Symptom evaluation is critical in identifying and managing potential neurological conditions, particularly those affecting aviation professionals. The thorough assessment of symptoms provides critical information for diagnosis and, subsequently, for determining the appropriate course of action. In the context of neurological conditions affecting pilots, symptoms can range from subtle cognitive changes to more pronounced motor impairments. These symptoms can significantly affect a pilot's ability to perform essential functions, including maintaining situational awareness, making critical decisions, and coordinating complex maneuvers. Early recognition and evaluation of these symptoms are vital for preventing potential accidents.
Recognizing the potential connection between symptoms and neurological conditions requires a nuanced understanding. For instance, subtle cognitive changes, such as difficulty with memory, attention, or problem-solving, might not be immediately apparent in everyday activities. However, these subtle changes can significantly impact a pilot's performance during flight. Similarly, motor coordination issues, even minor ones, can have severe implications in a high-stress, high-stakes environment like an airplane cockpit. Careful observation of such symptoms over time, often in combination with performance monitoring, is critical in detecting potential issues early. Case studies of pilots with undiagnosed neurological conditions highlight how seemingly minor symptoms, if unaddressed, can lead to safety risks and, in extreme cases, catastrophic outcomes.
Effective symptom evaluation in this context necessitates a multi-faceted approach. Physicians specializing in aviation medicine play a crucial role. This expertise encompasses not just the identification of symptoms but also an understanding of how those symptoms manifest in the unique environment of the cockpit. A thorough medical history, coupled with detailed assessments of cognitive and motor function, helps determine the potential impact on flight safety. Ongoing monitoring of performance, coupled with careful symptom evaluation, allows for early detection of emerging or worsening conditions. This proactive approach ensures that pilots who may be experiencing neurological issues receive appropriate medical attention and support, preventing potential flight hazards. The ultimate goal is to ensure safe flight operations by recognizing and addressing potential neurological impairment early in its progression.
4. Cognitive Function
Cognitive function encompasses a wide array of mental processes, including attention, memory, language, problem-solving, and decision-making. These functions are critical for safe and efficient flight operations. Compromised cognitive function can significantly impact a pilot's ability to perform complex tasks, make rapid decisions, and respond appropriately to unexpected situations in the cockpit. Conditions affecting cognitive function, sometimes referred to as "atpl brain disease," can pose significant safety risks, potentially leading to accidents or incidents. The intricacy and subtle nature of cognitive impairment make pre-flight screening and ongoing monitoring essential.
The importance of cognitive function in aviation stems from the inherent demands of piloting. Maintaining vigilance, processing information rapidly, and responding effectively to changing circumstances are paramount. Impaired cognitive function, resulting from conditions like dementia or certain types of stroke, can manifest in reduced alertness, decreased attention span, impaired judgment, and difficulty with problem-solving all critical for safe flight operations. Specific examples include pilots experiencing difficulty in recalling procedures during critical phases of flight or misjudging distance or speed. Early detection and management of cognitive impairments are crucial to prevent incidents. Furthermore, individuals exhibiting subtle changes in cognitive function may not readily recognize the issue themselves, highlighting the need for comprehensive medical evaluations and regular assessments to ensure pilot fitness for duty.
Understanding the connection between cognitive function and potential neurological conditions impacting aviators is crucial for aviation safety. This understanding underscores the importance of proactive health assessments, not just for the well-being of the pilot, but for the safety of passengers and the integrity of the operation. Continuous monitoring and proactive interventions can contribute significantly to mitigating the risks associated with impaired cognitive function and, thus, maintain safety standards in aviation. Regular cognitive assessments, coupled with rigorous pilot training and operational procedures, create a system that fosters a culture of safety, mitigating the potential for accidents stemming from these conditions.
5. Motor Skills
Motor skills, encompassing the execution of voluntary movements, are integral to safe piloting. Impairment in these skills, often a manifestation of underlying neurological conditions, presents significant safety risks. Precise, coordinated movements are crucial for tasks like controlling aircraft, operating flight controls, and executing maneuvers. Any deviation from expected performance can have serious consequences.
- Precise Control and Coordination
Maintaining precise control of the aircraft's flight path requires a high degree of motor coordination. Conditions impacting this coordination, such as tremors, muscle weakness, or incoordination, can significantly impair a pilot's ability to execute tasks accurately. This becomes especially critical during emergency situations, when rapid, precise control is vital. Examples of such conditions include Parkinson's disease, stroke, and multiple sclerosis, which can disrupt the neural pathways responsible for these precise movements. The impact on piloting is undeniable: inaccurate responses to controls can lead to unwanted maneuvers or even loss of control.
- Reaction Time and Speed
Prompt responses to changing situations are critical in the cockpit. Reduced reaction time, a common symptom of some neurological conditions, can hinder a pilot's ability to react to unexpected events or emergencies. This delay can lead to a cascading effect, further impacting flight safety. For instance, impaired reflexes or slow response times might lead to delayed or inappropriate adjustments of flight controls. Conditions like traumatic brain injury or certain neurological degenerations can significantly affect reaction speed, increasing the risk of accidents.
- Fine Motor Skills and Precision
Many flight tasks, such as adjusting instrument panels or operating complex controls, demand fine motor skills. Conditions affecting these small, precise movements can create limitations. For example, the inability to manipulate knobs or levers accurately or experience impaired dexterity can lead to missed controls or unintentional malfunctions. Conditions such as peripheral neuropathy or certain types of muscular dystrophy can lead to progressively diminishing fine motor capabilities, posing significant risks to flight safety.
- Impact of Disease Progression
Neurological conditions often progress over time. This progression can lead to a gradual decline in motor skills, potentially escalating safety concerns. Initial, barely noticeable impairments might not significantly impact everyday life but can become acutely detrimental in the exacting environment of the cockpit as the condition advances. Regular monitoring and adaptation of tasks are crucial in managing these conditions for continued safety. The subtle, evolving nature of these declines necessitates ongoing assessment and potentially modifying roles.
In summary, impaired motor skills, often linked to neurological conditions, represent a substantial safety concern in aviation. Understanding the various ways motor function can be compromised and the consequences for flight safety is crucial for establishing robust screening, monitoring, and management procedures for aviation personnel.
6. Sensory Perception
Sensory perception plays a critical role in piloting, encompassing the ability to accurately interpret and respond to visual, auditory, and other sensory information. Impairments in sensory perception, often resulting from neurological conditions, pose significant safety risks in aviation. Accurate perception of the surrounding environment and instruments is paramount. Deficiencies in this area can lead to misinterpretations of critical data or poor responses to immediate situations, potentially jeopardizing flight safety. Thus, understanding the relationship between sensory perception and neurological conditions is essential.
- Visual Perception
Visual acuity, depth perception, and the ability to discern colors and patterns are vital in aviation. Neurological conditions can affect these capabilities. For instance, conditions impacting the optic nerves or visual processing centers of the brain might lead to blurry vision, difficulties in judging distance, or trouble distinguishing crucial visual cues such as runway markings or instrument readings. These issues can have severe consequences during critical flight phases, particularly when navigating complex visual environments or interpreting instrument displays.
- Auditory Perception
Precise interpretation of auditory cues, such as engine sounds, communication signals, and external noises, is crucial for safe flight. Conditions affecting the auditory processing system can lead to difficulty distinguishing or localizing crucial sounds. For example, a pilot with impaired auditory processing might miss critical radio transmissions or fail to recognize subtle changes in engine noises that could indicate a problem. These limitations could impact crucial emergency responses, navigation decisions, and communication with air traffic control.
- Spatial and Kinesthetic Perception
Spatial awareness and the body's sense of position and movement (kinesthesia) are critical for maintaining stable flight and performing maneuvers. Neurological conditions can impair this complex interplay, causing a pilot to misjudge their aircraft's position or movement relative to the surrounding environment. Consequently, spatial disorientation or poor sense of aircraft control may arise, increasing the likelihood of errors and accidents. These sensory processing difficulties can lead to situations where the pilot misjudges the aircraft's altitude, speed, or position, potentially culminating in serious incidents.
- Other Sensory Inputs
While vision and hearing are paramount, other sensory inputs, such as touch and proprioception, contribute to the overall situational awareness. Neurological damage might cause issues with these less emphasized but critical senses, such as the tactile feedback from controls or the body's awareness of its own position. Any impairment in these senses can contribute to a less accurate understanding of the aircraft's condition, increasing the risk of misjudgments and mistakes.
In conclusion, sensory perception is a multifaceted component of pilot fitness. Conditions affecting sensory input pathways can severely compromise a pilot's ability to accurately perceive and react to essential flight information. Therefore, meticulous evaluation and ongoing monitoring of sensory perception are crucial for maintaining aviation safety and ensuring that individuals with neurological conditions are adequately supported, while considering their fitness for duty and the well-being of the flying public.
7. Regulatory Standards
Regulatory standards play a critical role in mitigating the risks associated with neurological conditions impacting aviation professionals. These standards, established to ensure flight safety, encompass pre-employment screening, ongoing medical evaluations, and procedures for managing pilots with diagnosed conditions. The effective implementation of these regulations is paramount in protecting the public and preserving the integrity of the aviation system. Failure to adhere to these standards can have severe consequences, as evidenced by past incidents involving pilots with undiagnosed or inadequately managed neurological conditions. Therefore, strong regulatory frameworks are essential to maintain safety standards and reliability in air travel.
Specific regulatory standards dictate medical certification requirements, outlining the criteria for assessing pilot fitness for duty. These requirements often include comprehensive neurological evaluations, including cognitive function tests, motor skill assessments, and evaluations of sensory perception. The standards also define procedures for managing pilots who have been diagnosed with neurological conditions. They may mandate periodic medical examinations, specify limitations on duty assignments, and detail processes for returning pilots to active service after treatment or rehabilitation. The standards also frequently include provisions for reporting suspected or confirmed neurological conditions, further emphasizing the importance of transparency and early detection. In essence, regulations act as safeguards, ensuring that individuals with conditions affecting their ability to pilot safely are identified and managed to prevent potential harm. Real-world examples demonstrate how non-adherence to these standards has led to accidents; hence, the strict adherence to them is crucial to maintain aviation safety.
In summary, regulatory standards are not simply guidelines; they are the cornerstone of aviation safety in the context of neurological conditions. Maintaining rigorous adherence to these standards, combined with proactive medical evaluations and monitoring, significantly reduces the risks associated with neurological issues affecting pilots. This approach safeguards passengers, crew, and the broader aviation community. The development and maintenance of robust regulatory frameworks provide a clear path forward in ensuring that appropriate procedures are in place for handling conditions and individuals with such conditions. These procedures minimize the potential for incidents arising from undiagnosed or inadequately addressed neurological concerns, effectively maintaining the overall safety of air travel.
8. Pilot Fitness
Pilot fitness is inextricably linked to the safety of flight operations and the well-being of passengers. Maintaining a high level of cognitive function, motor skills, and sensory acuity is crucial for safe piloting. Conditions impacting these areas, such as those potentially encompassed by the term "atpl brain disease," pose significant risks. Comprehensive evaluation of pilot fitness is essential to address and mitigate the potential for incidents stemming from these conditions.
- Pre-Employment Screening and Certification
Rigorous pre-employment screening processes are fundamental for ensuring pilots are fit for duty. These evaluations aim to identify individuals with neurological conditions that might compromise their abilities, ensuring they do not enter the profession with concealed or undiagnosed impairments that could pose risks. This process includes medical assessments focused on cognitive function, motor skills, and sensory perception, helping to identify potential vulnerabilities early. This preventative measure reduces the likelihood of individuals with underlying conditions entering the pilot training pipeline.
- Ongoing Medical Evaluations and Monitoring
Ongoing medical evaluations and monitoring are necessary to detect subtle changes in a pilot's capabilities. As neurological conditions can evolve gradually, regular health assessments are essential to identify and address potential impairments in time. These evaluations go beyond basic health checks, often incorporating cognitive tests, motor skill evaluations, and assessments of sensory processing. This ongoing monitoring allows for early intervention and adaptation of procedures, minimizing risks before they escalate into safety concerns.
- Assessment of Specific Conditions
Specific neurological conditions demand tailored assessments, accounting for their distinct effects on cognitive function, motor skills, and sensory perception. The evaluation process for pilots suspected of, or diagnosed with, conditions that might impact their fitness for duty must consider the specific challenges and limitations posed by the condition. This includes understanding how these conditions can affect judgment, response time, and coordination, which are critical for safe piloting. Specialized testing and expert consultations may be necessary to fully evaluate potential limitations and inform decisions about pilot fitness for duty.
- Adaptation of Tasks and Duty Assignments
Adaptive measures, such as adjusting task assignments or limiting certain flight operations, are often necessary for pilots with existing or developing neurological conditions. This proactive approach ensures pilots are not exposed to situations where their impairments could compromise safety. These adjustments could include limiting complex maneuvers, reducing exposure to high-stress situations, or adapting training programs to meet specific needs. Such adaptations can preserve both pilot safety and the safety of air travel.
In conclusion, maintaining pilot fitness is not just a regulatory requirement; it is a crucial aspect of ensuring the safety and reliability of air travel. The comprehensive approach to pilot fitness, encompassing pre-employment screening, ongoing monitoring, specialized evaluations for specific conditions, and adaptable duty assignments, forms a layered defense against the risks associated with neurological conditions. This multifaceted system aims to maintain high standards of aviation safety by proactively identifying and addressing potential vulnerabilities and ensures that only fit-for-duty pilots are entrusted with the critical responsibility of operating aircraft.
Frequently Asked Questions about Neurological Conditions Affecting Aviation Professionals
This section addresses common questions and concerns regarding neurological conditions that may impact aviation professionals. Accurate information and understanding are essential for ensuring flight safety and the well-being of all involved.
Question 1: What are some of the most common neurological conditions that might affect aviators?
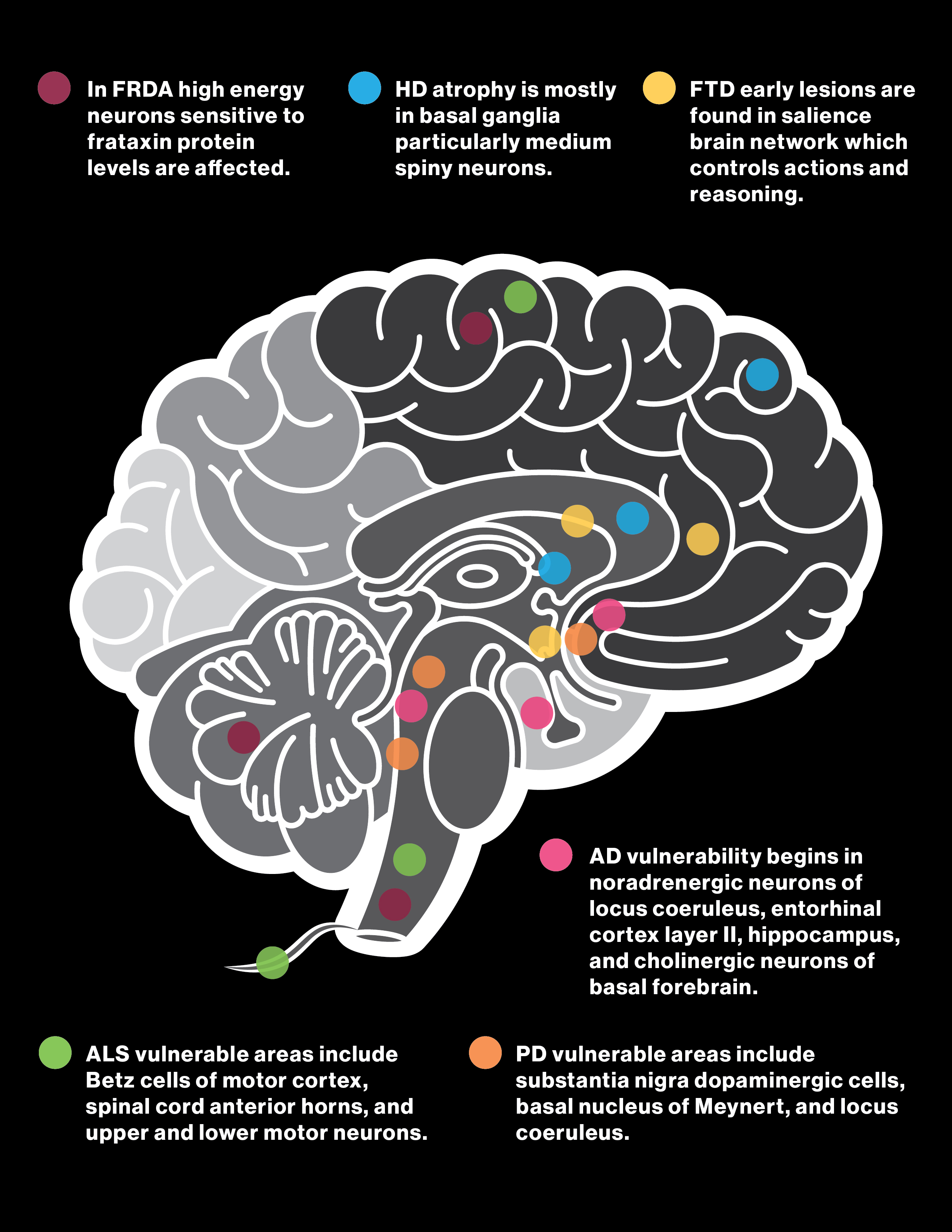
Several neurological conditions can impact an aviator's performance. Examples include, but are not limited to, various types of cognitive impairment, such as dementia or stroke; movement disorders like Parkinson's disease or multiple sclerosis; and sensory processing difficulties. The specific impact depends on the condition's severity and nature. These conditions can affect attention, memory, decision-making, motor skills, and sensory interpretation, all crucial for safe flight operations. It is important to note that many conditions can manifest gradually, making early detection challenging.
Question 2: What are the implications of these conditions for flight safety?
Compromised cognitive function, motor skills, or sensory processing can severely impact a pilot's ability to perform their duties safely. This includes issues with reaction time, spatial awareness, complex decision-making, and maintaining vigilance. Difficulties in these areas can lead to misjudgments, errors in critical procedures, and poor responses during emergencies, posing significant risks to the pilot, passengers, and the aircraft. Early detection and management are crucial.
Question 3: How are these conditions diagnosed?
Diagnosis relies on a comprehensive evaluation, often involving a detailed medical history, physical examination, and specialized neurological tests. These tests may include assessments of cognitive function, motor skills, and sensory perception. Evaluations consider the individual's specific job demands, helping determine the potential impact on flight operations.
Question 4: What are the management strategies for these conditions?
Management strategies are individualized and depend on the specific condition and its progression. Strategies may involve medication, therapy, lifestyle adjustments, and adaptations to operational duties. Ongoing monitoring and adjustments to responsibilities are often necessary.
Question 5: What is the role of regulatory bodies in addressing these issues?
Regulatory bodies play a vital role in establishing and enforcing standards for pilot fitness. These standards typically involve pre-employment screening, periodic medical evaluations, procedures for managing pilots with diagnosed conditions, and return-to-duty criteria. These regulations aim to ensure only fit-for-duty aviators operate aircraft, thus maintaining safety standards. Regulatory frameworks vary depending on jurisdictions.
Understanding the potential impact of neurological conditions on aviation professionals is crucial for fostering safety in flight operations. The interplay of medical evaluation, regulatory standards, and individualized management strategies is key to preventing incidents and maintaining public trust. This requires vigilance, effective communication, and adherence to established protocols.
The following sections will explore specific diagnostic criteria and management strategies in more detail.
Conclusion Regarding Neurological Conditions Affecting Aviation Professionals
This article explored the multifaceted challenges posed by neurological conditions, often encompassing the spectrum of impairments broadly categorized under "atpl brain disease," within the aviation profession. Key findings highlighted the critical interplay between robust regulatory frameworks, comprehensive medical evaluations, and individualized management strategies in maintaining flight safety. The intricate nature of these conditions, characterized by varied presentations, gradual progression, and potential for subtle but significant impairments, necessitates a meticulous approach to pilot fitness. The article underscored the importance of pre-employment screening, ongoing monitoring, and specific adaptation of duties for aviators with diagnosed or suspected neurological conditions. A concerted effort to accurately diagnose these conditions in their early stages is critical to mitigating risks associated with impaired cognitive function, motor skills, and sensory perception. Historical examples demonstrate how negligence in these areas can lead to severe consequences.
Maintaining the highest standards of aviation safety requires a commitment to comprehensive, proactive measures. This includes stringent adherence to regulatory standards, the ongoing development and application of advanced diagnostic tools, and continued investment in training programs that focus on recognizing and managing neurological conditions in aviators. A culture of vigilance, transparency, and shared responsibility among medical professionals, regulatory bodies, and aviation personnel is indispensable. The overarching objective is to ensure that only pilots capable of consistently and safely performing their complex duties are entrusted with the critical task of operating aircraft, thus protecting the well-being of passengers and crew while maintaining the integrity of the aviation system.
Article Recommendations
- Betty Claire Kalb Gene Barry Love Story Legacy Uncovered
- Amber Stevens West Latest News Updates You Need To Know

Detail Author:
- Name : Dr. Joanie Larkin I
- Username : jkuhic
- Email : lilyan.grady@stokes.info
- Birthdate : 2001-12-20
- Address : 73540 Hickle Flat New Pearlieport, WY 02197
- Phone : (828) 900-8629
- Company : Streich-Hill
- Job : Therapist
- Bio : Nostrum voluptatem dolorum est facere et consectetur sunt. Eum dolores rerum eveniet provident ad voluptates. Qui et voluptatem porro delectus.
Socials
tiktok:
- url : https://tiktok.com/@noah_official
- username : noah_official
- bio : Ut cum at laborum magni accusamus.
- followers : 349
- following : 733
linkedin:
- url : https://linkedin.com/in/noah6702
- username : noah6702
- bio : Quo dolorem fuga ratione nam.
- followers : 290
- following : 1674
twitter:
- url : https://twitter.com/volkman1972
- username : volkman1972
- bio : Voluptatem rerum odit quis ipsam. Sit rerum nisi molestiae quaerat cumque distinctio dolores. Minus repellat ut aliquam quo. Ea veritatis itaque placeat ea.
- followers : 365
- following : 2706
facebook:
- url : https://facebook.com/volkman2008
- username : volkman2008
- bio : Libero molestiae aspernatur explicabo commodi corrupti eum.
- followers : 1689
- following : 1980